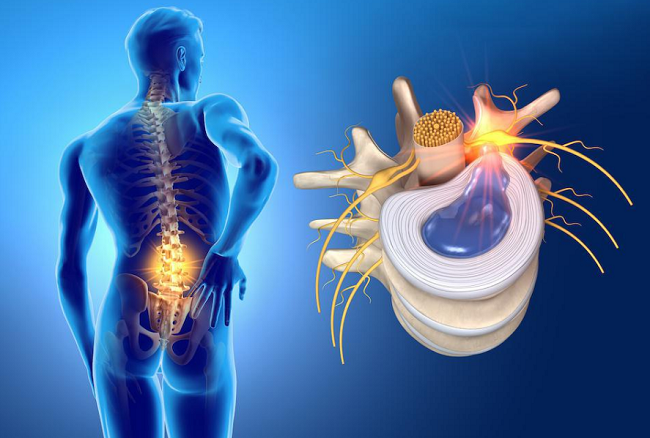
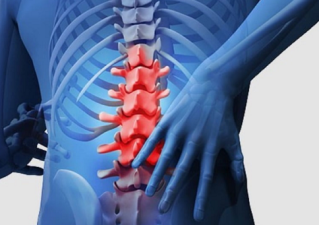
A herniated disc, often the source of back pain, numbness, or weakness, requires careful diagnosis to ensure effective treatment. Diagnostic tools range from imaging technologies such as X-rays, MRI scans, and CT scans to codes for medical records and disability assessments. This blog post aims to navigate these complex realms of herniated disc diagnosis, making them more accessible and understandable for everyone.
How is a Herniated Disc Diagnosed?
The process of diagnosing a herniated disc typically starts with a physical exam and a review of your medical history. Your healthcare provider may ask you about your symptoms, their severity, and any factors that worsen or improve them. They may also perform a neurological examination to check your reflexes, muscle strength, and sensory responses. If a herniated disc is suspected, imaging tests are usually ordered to confirm the diagnosis and assess the condition’s specifics.
- X-rays: While X-rays do not directly visualize the discs (they only show bones), they can help rule out other conditions that may cause similar symptoms. Specific herniated disc X-ray findings may include reduced disc space or bone spurs.
- MRI Scans: As discussed in our previous blog post, MRI is the gold standard for visualizing herniated discs. It provides detailed images of the spine, allowing for precise localization and assessment of herniations.
- CT Scans: A CT scan can also provide detailed images of the spine, helping to detect herniated discs, particularly in patients who cannot undergo MRI.
- Ultrasound: Though not commonly used for diagnosing herniated discs, ultrasound technology is being explored as a potential tool, particularly for assessing patients who cannot undergo MRI.
Understanding Medical Codes: ICD-10 and ICD-9
The International Classification of Diseases (ICD) is a system used worldwide to standardize the coding of medical conditions. The codes for herniated discs in the ICD-10 (current version as of the time of writing) start with M51, followed by a decimal and further digits to specify the disc’s location and whether any nerve compression is present.
The previous version, ICD-9, also had specific codes for herniated discs, usually starting with 722. The transition from ICD-9 to ICD-10 has allowed for more specific and detailed coding of medical conditions.
Herniated Disc Sizes: What Do They Mean?
When you read your diagnostic report, you might see measurements in millimeters (mm) describing the size of the herniated disc. This measurement usually represents the extent of disc material displacement. The significance of the size of a herniation varies – a small herniation (like a 3mm or 4mm herniated disc) can cause significant symptoms if it’s pressing on a nerve, while a larger herniation (like a 9mm or 12mm herniated disc) might cause few or no symptoms if it’s not impinging on any neural structures.
Herniated Disc Disability Rating
If a herniated disc results in long-term impairment, you might receive a disability rating. This rating, expressed as a percentage, represents the extent of the disability caused by the condition. The exact rating can depend on various factors, including the severity of the herniation, the level of functional limitation, and the impact on the person’s ability to perform daily activities or work tasks.
Home Testing for Herniated Discs
While formal diagnosis should always be made by a healthcare professional, some tests can be done at home to indicate if a herniated disc may be causing your symptoms. These could include maneuvers that increase intra-abdominal pressure (like coughing or sneezing) or certain positions or movements that provoke your symptoms.
Provoking Symptoms at Home: What to Watch For
One example of a home test for a herniated disc is the straight leg raise test. Here’s how you do it: Lie down on your back on a flat surface. Keeping your leg straight, lift it slowly off the surface. If this movement causes pain that radiates down your leg, it could indicate a herniated disc.
Another test you could try is to walk on your toes and then on your heels. Difficulty with this simple task could suggest a herniated disc.
While such tests can suggest the presence of a herniated disc, they are not definitive. If these tests produce pain or if your symptoms persist, it’s essential to seek medical attention. A healthcare provider can perform more thorough examinations and order appropriate imaging tests to confirm the diagnosis and rule out other possible causes of your symptoms.
When Size Matters: Understanding Herniated Disc Sizes
The size of a herniated disc can have different implications, depending on its location and whether it’s impinging on any nerves. In the lumbar spine, for instance, a 6mm herniated disc at the L4-L5 level could potentially press on the L5 nerve root, possibly causing symptoms like lower back pain, numbness or tingling in the leg, and possibly weakness in certain leg muscles.
A 9mm herniated disc, while larger, may not necessarily cause more severe symptoms than a smaller herniation if it’s not pressing on any crucial structures. Conversely, a 12mm herniated disc is considered large and is more likely to cause significant symptoms or nerve compression.
However, it’s important to remember that the size of the herniation doesn’t always correlate with the severity of symptoms. Some people with large herniations may have few symptoms, while others with small herniations may experience significant pain and disability. Treatment decisions are usually based not just on the size of the herniation, but also on the patient’s symptoms, overall health, and response to conservative treatments.
In Conclusion
Diagnosing a herniated disc involves a comprehensive evaluation including a physical examination, a review of your symptoms and medical history, and various diagnostic tests. Understanding these processes, and the role of diagnostic tools like X-rays, MRIs, CT scans, and even home tests, can help you participate more actively in your care. Despite the complexity of these diagnostics, remember that your healthcare provider is there to guide you and make sense of all the information. With their help, you can navigate the path to recovery from a herniated disc.
Chiropractic Treatment for Herniated Discs
The approach of chiropractic treatment for herniated discs is typically holistic and patient-centered, aiming to provide relief without surgical intervention or drugs.
Spinal Manipulation: This is the most well-known chiropractic technique, also called chiropractic adjustment. The chiropractor applies a controlled, sudden force to the affected spinal joint, which may help to align the spine, improve spinal function, and alleviate pain. This technique, when done correctly by a professional, is considered safe but should not be performed if certain contraindications exist, like severe osteoporosis or spinal cancer.
Flexion-Distraction Technique: This is a gentle, non-thrust type of spinal manipulation often used for herniated disc treatment. The chiropractor uses a special table that distracts or stretches the spine, and by using a pumping action on the disc instead of direct force, the pressure on the disc can be reduced, leading to pain relief.
Pelvic Blocking Techniques: These methods involve placing cushioned wedges on the sides of the patient’s pelvis, along with gentle stretches. This can help move the disc away from the nerve, reducing inflammation and pain.
Physical Therapy Modalities: Many chiropractors also employ physical therapy techniques, such as ice and heat therapy, electrical stimulation, or ultrasound to reduce inflammation and muscle spasm associated with herniated discs.
Exercises and Lifestyle Modifications: A chiropractor can provide exercises tailored to the patient’s condition, which can help strengthen the spinal muscles and prevent further injury. They may also offer advice on posture and ergonomics to help prevent disc herniation in the future.