Sciatica is a common condition that affects many people, causing pain, numbness, and tingling in the lower back, buttocks, and legs. One of the primary causes of sciatica is a herniated disc, which can compress or irritate the sciatic nerve. In this article, we will discuss the relationship between herniated discs vs sciatica, the symptoms of both conditions, and the available treatment options.
Herniated Disc or Sciatica: The Connection
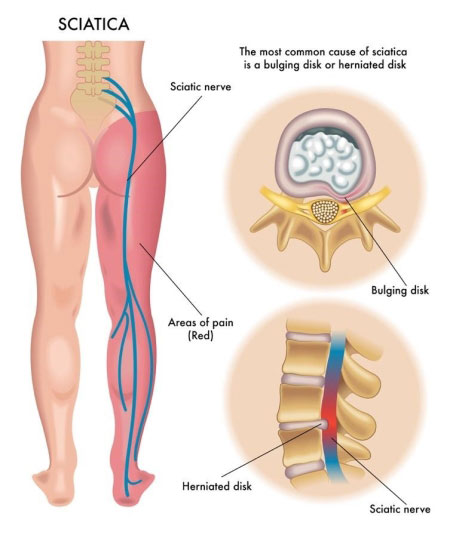
Sciatica is a symptom that results from the compression or irritation of the sciatic nerve, the longest and largest nerve in the body. A herniated disc, also known as a ruptured or slipped disc, occurs when the soft inner core of an intervertebral disc (the nucleus pulposus) pushes through a tear in the tough outer layer (the annulus fibrosus).
When a herniated disc compresses or irritates the sciatic nerve, it can lead to sciatica symptoms, such as pain, numbness, and tingling in the lower back, buttocks, and legs. It’s essential to recognize that sciatica is not a standalone condition but a symptom of an underlying issue like a herniated disc.
Herniated Disc or Pinched Nerve
A pinched nerve can also cause symptoms similar to those of sciatica. When a nerve is compressed or “pinched” due to factors such as inflammation, injury, or spinal degeneration, it can result in pain, numbness, and tingling. While a herniated disc is a common cause of a pinched nerve, other conditions, such as spinal stenosis or spondylolisthesis, can also lead to nerve compression.
Herniated Disc Nerve Pain
Nerve pain resulting from a herniated disc can manifest in various ways, depending on the location of the herniation and the specific nerve affected. Common symptoms of herniated disc nerve pain include:
- Sharp, shooting pain in the neck, back, or extremities
- Numbness, tingling, or weakness in the arms or legs
- Muscle spasms or cramps
Treatment for Herniated Disc and Sciatica
Treatment for both herniated discs and sciatica typically begins with conservative measures, such as:
- Rest and activity modification: Avoiding activities that worsen symptoms and incorporating gentle movements to promote healing
- Over-the-counter pain relievers and anti-inflammatory medications: To help manage pain and reduce inflammation
- Physical therapy: Strengthening and stretching exercises to support the spine, improve posture, and alleviate pressure on the sciatic nerve
- Chiropractic care or spinal manipulation: To help realign the spine and reduce nerve compression
- If conservative treatments are unsuccessful or if neurological symptoms worsen, more invasive options may be considered, such as:
- Epidural steroid injections: Delivering anti-inflammatory medication directly to the affected area to reduce inflammation and relieve pain
- Surgery: In severe cases, a surgical intervention like a discectomy or spinal fusion may be necessary to remove the herniated disc material and stabilize the spine
Conclusion
Understanding the connection between herniated discs and sciatica is crucial for accurate diagnosis and appropriate treatment. Both conditions can cause significant pain and discomfort, impacting daily life and overall well-being. By working closely with healthcare professionals and following a personalized treatment plan, individuals with herniated discs and sciatica can work towards long-term pain relief and recovery. Early intervention, including conservative measures like medication, rest, and physical therapy, can help manage symptoms and promote healing, while more invasive interventions may be necessary in severe cases.